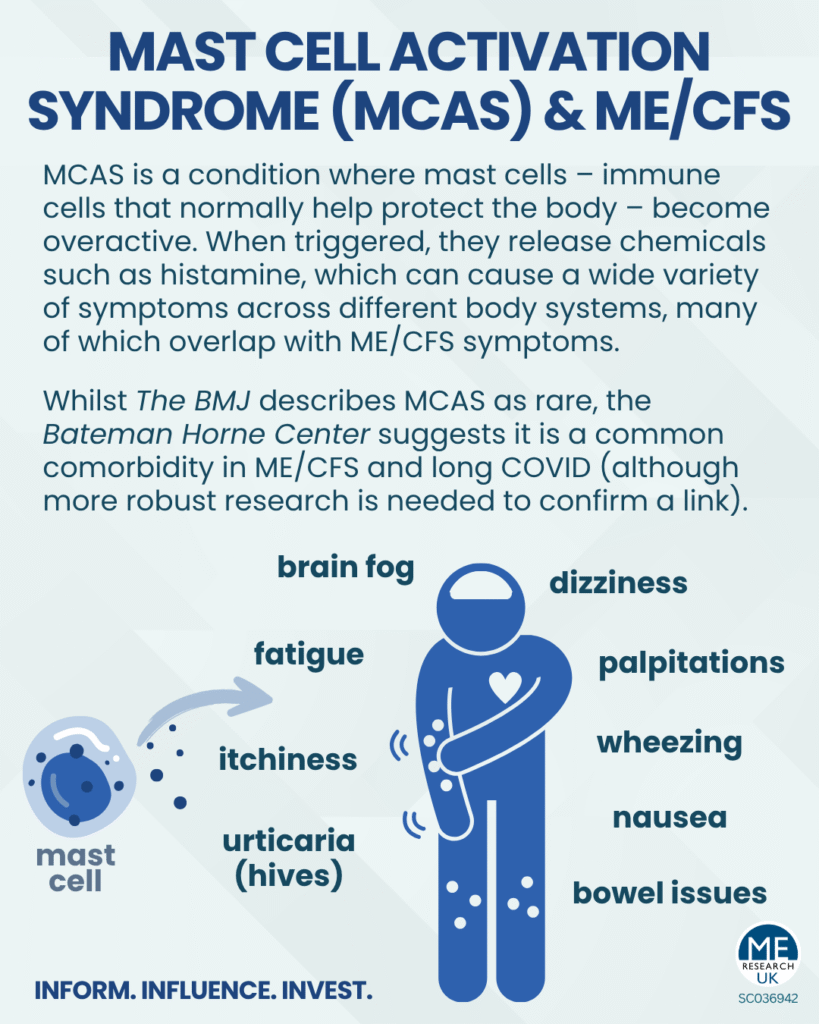
Mast cell activation syndrome (MCAS) is a condition where mast cells – immune cells that normally help protect the body – become overactive. When triggered, they release chemicals such as histamine, which can cause a wide variety of symptoms across different body systems, many of which overlap with ME/CFS symptoms. It is thought that activation of mast cells can contribute towards symptoms of dysautonomia (dysfunction of the autonomic nervous system).
Whilst BMJ Best Practice describes MCAS as rare, the Bateman Horne Center suggests it is a common comorbidity in ME/CFS and long COVID (although there currently is no robust research to confirm a link between ME/CFS and MCAS). It is also possible that MCAS is underdiagnosed, since its symptoms are broad and often mistaken for other conditions.
Symptoms
MCAS can affect many parts of the body. Common symptoms include:
- Skin: flushing, urticaria (hives), itching
- Heart and circulation: palpitations, chest pain
- Lungs: coughing, wheezing
- Gut: nausea, vomiting, diarrhoea, constipation, throat tightness, difficulty swallowing
- General / brain-related: fatigue, dizziness, brain fog, lightheadedness
- Severe: in some cases, anaphylaxis (a serious allergic-type reaction)
Common triggers
Often-identifiable triggers vary between individuals, and commonly include:
- Infections
- Temperature changes
- Certain foods (especially high-histamine foods)
- Alcohol
- Medications (e.g. NSAIDs)
- Sunlight
- Stress
What does the research say?
So far, research linking MCAS and ME/CFS is limited:
- One review noted that a direct association between MCAS and ME/CFS appears infrequent. However, it stated “Nevertheless, there is clear evidence for a role of histamine and allergic predisposition in ME/CFS and long COVID. The most convincing evidence for the involvement of histamine is the alleviating action of long-term symptoms of post-COVID-19 infection upon the anti-histamine treatment.”
As we know, for a proportion of individuals with long COVID, the COVID-19 virus triggered ME/CFS. - The researchers also proposed linked mechanisms between MCAS, ME/CFS, postural orthostatic tachycardia syndrome (PoTS), decreased cerebral blood flow, and small fiber neuropathy (SFN). They suggest that all of these may involve:
- Over-release of inflammatory and vasoactive (affecting blood vessel diameter) molecules/substances
- Dysfunction of certain cell receptors (β2-adrenergic receptors)
- Another study suggested that COVID-19 infection might worsen existing undiagnosed MCAS, possibly explaining why some individuals with long COVID experience symptoms that could suggest MCAS.
Diagnosis
MCAS can be difficult to diagnose because the symptoms overlap with other conditions. Healthcare professionals may additionally look for:
- A rise in mast cell markers (such as serum tryptase) during episodes
- Symptom improvement with medications that target mast cells
Management
Treatment usually focuses on:
- Avoiding known triggers e.g. minimising stress, following a low-histamine diet
- Medications such as:
- Antihistamines (H1 and H2 blockers)
- Leukotriene receptor antagonists
- Mast cell stabilisers
Emergency treatment with adrenaline (epinephrine) is needed for severe reactions such as anaphylaxis.
Conclusion
Whilst MCAS and ME/CFS are not the same condition, there is an overlap in symptoms and potentially in biological pathways. For individuals with ME/CFS who suspect co-occurring MCAS, it may be worth exploring with a healthcare provider, as treatment for MCAS may reduce the overall burden of symptoms.
As this article states, evidence and research on MCAS in relation to ME/CFS is sparse. Any interaction between the two conditions is not well understood and appears to be complex. This article is provided as part of Dysautonomia Awareness Month with MCAS falling within that broad umbrella of illnesses and not intended as a full exploration of MCAS nor MCAS and ME/CFS.