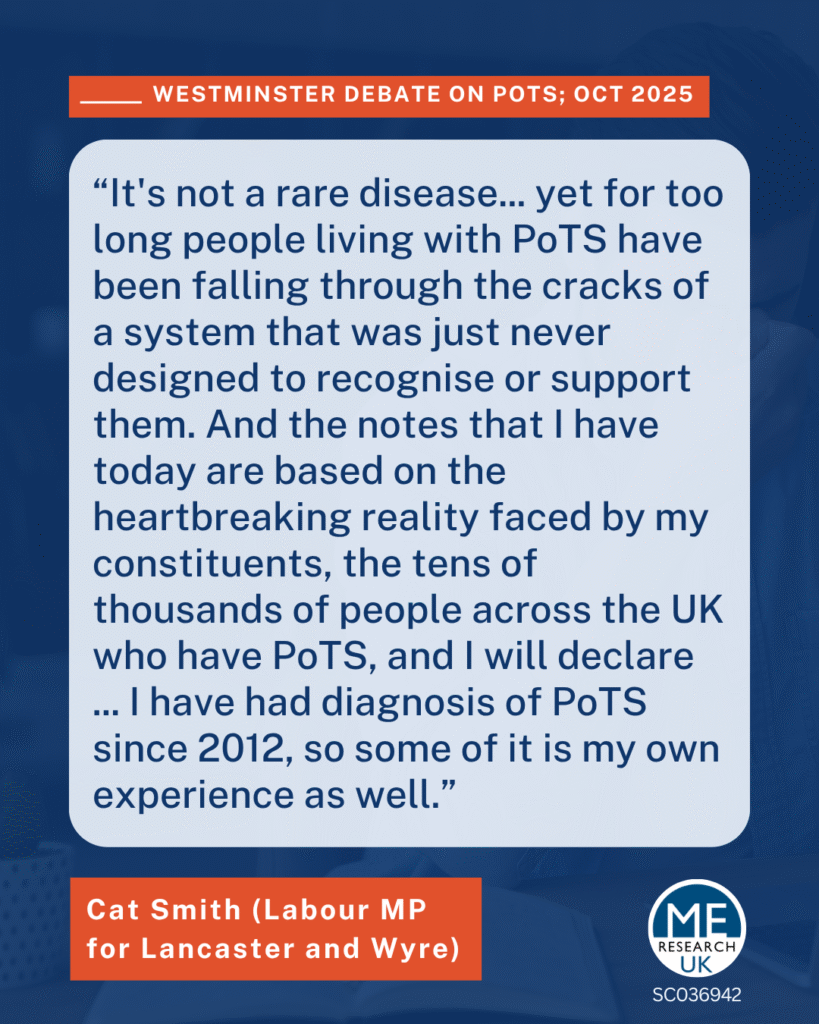
Labour MP for Lancaster and Wyre, Cat Smith, led the Westminster debate on postural orthostatic tachycardia syndrome (PoTS) emphasising that PoTS is not a rare disease, yet individuals with PoTS are “falling through the cracks” of a healthcare system unprepared to recognise or support them. Drawing on her own experience and those of constituents across the UK, she called for urgent reform in diagnosis, treatment, and care pathways for people with PoTS. Minister Ashley Dalton responded during the session that lasted around half an hour.
Overview of MP Cat Smith’s speech
1. Diagnostic delays and disbelief
- The average time to diagnosis is seven years – “one of the first… and longest fights” individuals with PoTS face.
- During this period, individuals are often disbelieved.
- The delay can lead to loss of education, employment, social isolation, and impact mental health.
- This is not likely due to doctors’ lack of care but because awareness of PoTS is “astonishingly low within the medical profession”
2. Shortage of expertise and overwhelmed services
- Few clinicians are trained in autonomic disorders (such as PoTS) “as a result patients often find themselves referred between different specialties”.
- In London, one major clinic has stopped accepting new patients and another is limiting care to locals, with rejected referrals going to a third London clinic that has a two-year waiting list.
- Access to diagnosis and care is a “postcode lottery” which “depends entirely on where you live”.
3. Systemic and structural failings
- These problems are “not simply matters of medical complexity” but result from a system “never built to recognise or support” people with PoTS.
- A surge in cases linked to long COVID has made the situation even more urgent.
- There is a fundamental lack in clinical understanding of the autonomic nervous system, “which sits awkwardly between medical disciplines and is often overlooked in medical education:.
4. Gender health gap
- PoTS predominantly affects women, and Cat Smith linked diagnostic delays to a wider gender bias in UK healthcare “where many women receive poorer healthcare than men”.
5. Calls for government action
Cat Smith welcomed the government’s 10-year plan, but questioned whether it would genuinely help individuals with PoTS since it “focuses heavily on prevention rather than diagnosis” which “isn’t a coherent strategy for chronic multi-system conditions like PoTS”. She made a five-point request to the Minister:
- National NICE guidelines to provide an evidence-based framework for diagnosis and treatment. She asked if there would be inclusion of PoTS training for frontline clinicians within new specialty training posts, and whether there will government investment in PoTS-specific research and initiatives.
- Require ICBs (Integrated Care Boards) to understand PoTS prevalence within their community and provide for the needs of these patients accordingly.
- Ensure every ICB has a clear clinical pathway that ensures patients access to regional specialist services, “not just central London” – ending the postcode lottery.
- Protect and support existing specialist clinics, which are “being overwhelmed and are under threat from closure by hospital management”.
- Designate PoTS and related disorders as a health and social care priority, ensuring equitable access to NHS healthcare and social support.
At the beginning of Cat Smith’s speech she took several interventions from MPs, representing constituents across the UK, who also highlighted how important raising the issue was.
Key themes from MP Interventions
1. Diagnosis delays and misdiagnosis
- MPs from across the UK described lengthy diagnostic delays and lack of specialists in their regions. Example: One MP stated, “in Northern Ireland, not only does it take seven years for diagnosis, but we do not, it appears, have a single PoTS specialist which is aggravating the situation.”
- It was noted that patients may be misdiagnosed with mental health conditions
2. Need for national clinical guidelines and care pathways
- Issues with referrals were pointed out and an “absence of national clinical guidelines and clear care pathways” leading to inadequate diagnostic processes.
3. Awareness and training for medical professionals
- MPs highlighted low awareness among medical professionals, with one MP stating “Most GPs will never have encountered the term in their training and even amongst cardiologists and neurologists. Expertise in [autonomic] disorders are scarce and as a result patients often find themselves referred between different specialities.”
- One MP shared a case where a consultant in Bristol told a patient that PoTS was a “TikTok fashion”.
- MPs called for more research related to PoTS.
4. Impact on individuals and families
- MPs shared stories of constituents enduring years of misdiagnosis and inadequate care. They described devastating effects on quality of life, including loss of employment, education, and independence.
- One MP stated, “… One of my constituents in Aylesbury has become a full-time carer to her 25-year-old son who is affected by PoTS, developed it at university, had to drop out, now is unable to work.”
- Repeated disbelief from clinicians and chronic illness itself severely affect mental health. Cat Smith agreed, saying “when you [are disbelieved] by medical professionals for so long it can affect your mental health.”
- One MP, stated that their constituent had resorted to going private for a diagnosis.
Overview of Minister Ashley Dalton’s response
Minister for Public Health and Prevention, Ashley Dalton, began by congratulating Cat Smith MP for “bringing this very important issue forward” and praised her passionate advocacy stemming from personal experience. She also acknowledged the interventions of MPs and thanked them for sharing their constituents’ stories, although stated that there would not be time in the short debate to respond to individual interventions.
Ashley Dalton stated that PoTS is not a rare condition, affecting an estimated 120,000 people in the UK, and that it is “a debilitating multi-system disorder that can significantly impact someone’s quality of life.” She accepted that individuals affected face misdiagnosis, delays, lack of specialist care, lack of understanding, and a postcode lottery.
On policy matters, the Minister:
- Accepted that there is a lack of national guidance but said developing formal NICE guidelines is difficult because of limited available evidence, the overlap with conditions such as long COVID and ME/CFS, and ” the fact that PoTS is often managed with lifestyle changes”.
- Mentioned that NICE already refers to PoTS in its summary on blackouts/syncope, and that information is available from PoTS UK and the International Heart Rhythm Society.
- Stressed that it is the responsibility of ICBs to providing local PoTS services, and said NHS England must hold them accountable when they fail to meet this statutory duty.
- Highlighted the government’s support for research through the NIHR, including investing £3 million into the LOCOMOTION study looking at the connection between long COVID and autonomic disorders, and invited new research proposals focused on PoTS.
- Agreed to meet with PoTS specialists to discuss systemic challenges and how to move forward.
- Linked the issue to broader government initiatives such as the 10-Year Health Plan and the ME/CFS delivery plan, stating “given that PoTS is frequently comorbid with ME/CFS the final delivery plan for ME/CFS which the government published this summer will have a positive impact for many PoTS patients too”.
- Emphasised that helping people with PoTS into work fits within wider government efforts to support people with long-term health conditions under the “Get Britain Working” strategy.
What could this mean for patients and campaigners?
The Minister’s response clearly recognised the daily struggles of people with PoTS and the systemic barriers they face. However, it did not announce any new funding, policy changes, or immediate interventions for overstretched clinics. Responsibility was largely deferred to local ICBs and future research outcomes.
In short, the response provided welcome recognition but limited action – a positive start in tone, but not yet the decisive, coordinated strategy that advocates seem to be asking for.