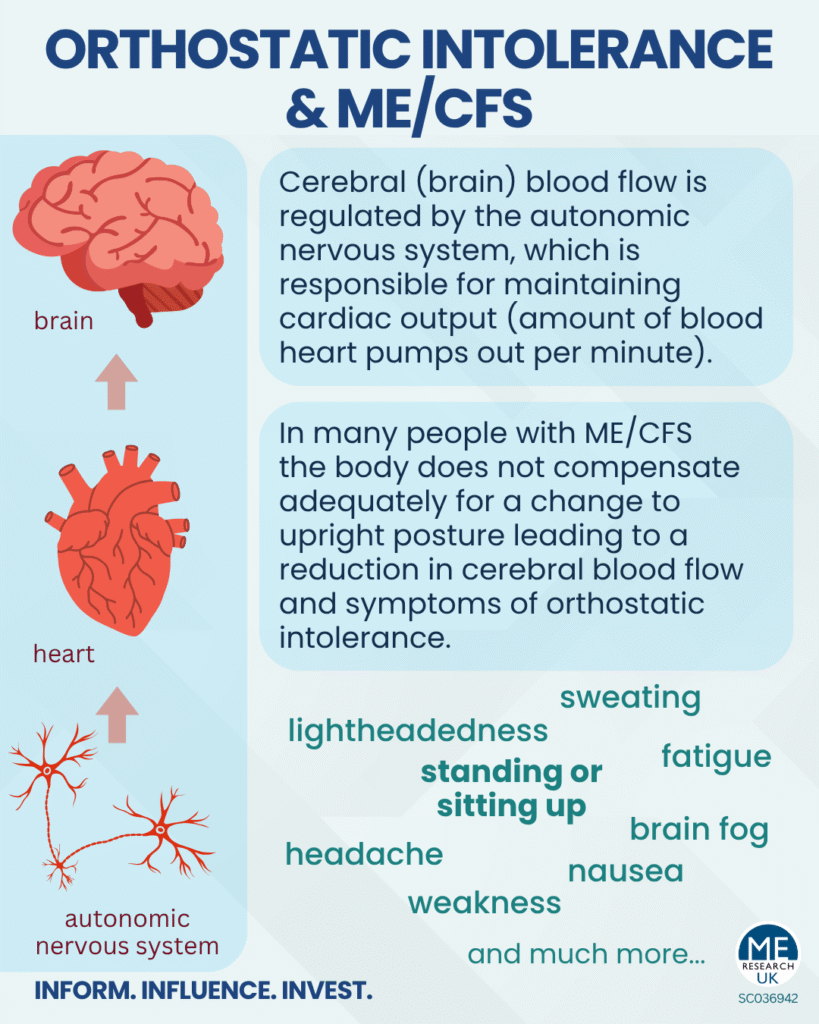
Orthostatic intolerance, a common issue for people with ME/CFS, refers to when the body fails to properly compensate for moving to an upright position, which is thought to result in reduced blood flow to the brain and symptoms such as lightheadedness, fatigue, and weakness. A subset of those with orthostatic intolerance also meet the criteria for postural orthostatic tachycardia syndrome (PoTS), which includes an excessive increase in heart rate as one of the symptoms.
Orthostatic intolerance can be a subcategory of dysautonomia (conditions that affect the autonomic nervous system).
ME Research UK has multiple articles on orthostatic intolerance, including:
Orthostatic intolerance, cerebral blood flow, and ME/CFS
When a healthy individual stands up, gravity pulls blood down towards the legs and abdominal area. In a healthy person, the body quickly compensates by tightening blood vessels (vasoconstriction), to maintain adequate blood supply to the brain. However, in many individuals with ME/CFS, this compensatory response is impaired, leading to reduced cerebral (brain) blood flow and orthostatic intolerance. It seems that this can occur, even in absence of an overall blood pressure drop like in orthostatic hypotension.
PoTS is a debilitating, under-recognised condition and co-morbidity of ME/CFS, characterised by an abnormal rise in heart rate, in addition to other symptoms, when a person transitions to an upright position. PoTS is thought to affect at least 0.2% of the general population and is more prevalent in females aged between 15 and 50, although it does occur in males.
In PoTS, compensatory responses (when standing up) to keep blood pressure and blood flow to the brain stable are thought to be dysregulated. In PoTS, the compensation (involving increasing heart rate and activation of the sympathetic nervous system) often seems to work just well enough to prevent a significant drop in blood pressure – but not necessarily well enough to fully preserve adequate blood flow to the brain.
ME/CFS, Orthostatic Intolerance, and the Tilt Table Test
Many individuals with ME/CFS have orthostatic intolerance, but not PoTS. During tilt table testing (gold standard test for PoTS), cerebral blood flow and the related cardiac output are not routinely measured. If routine measurement were to occur abnormalities in cerebral blood flow related to orthostatic intolerance are likely to be noted more often.
Heat, ME/CFS and orthostatic intolerance
Many factors can worsen orthostatic intolerance, but heat is a particularly relevant trigger during the summer months.
Orthostatic Intolerance in ME/CFS and long COVID
Researchers believe that a simple orthostatic stress test should be performed in doctors’ offices to assess the impact of long COVID and ME/CFS on blood pressure, balance, cognitive abilities and general health.
Can treatment for individuals with ME/CFS and PoTS be more targeted?
Researchers noted two subgroups amongst individuals with ME/CFS and concurrent PoTS. In those with a limited heart rate increase, mainly increased accumulation of blood (particularly in lower limbs) was observed. In those with a larger heart rate increase (over 40 beats per minute), the data showed exaggerated activation of the sympathetic nervous system. According to the researchers, this opens the door to the possibility of tailoring PoTS treatments according to the profile.
BH4 upregulation in people with ME/CFS and orthostatic intolerance
A pilot study found that participants with ME/CFS who also had orthostatic intolerance had increased levels of a molecule named BH4.