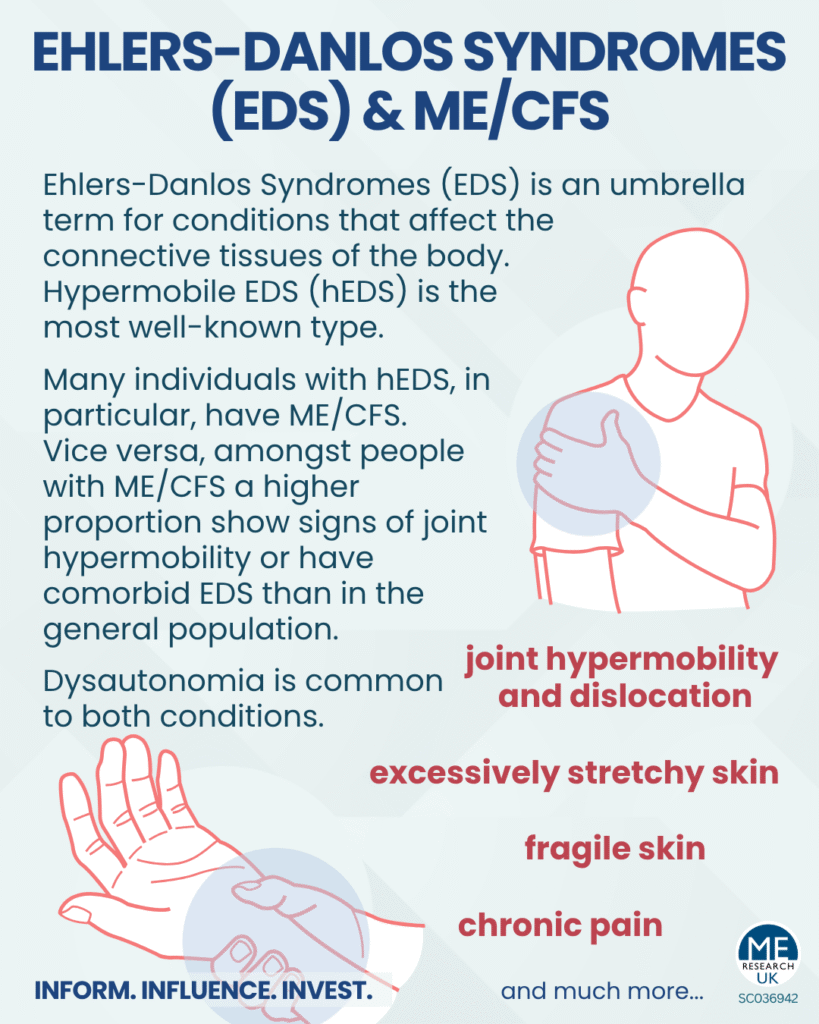
Ehlers-Danlos Syndromes (EDS) is an umbrella term for a group of conditions that affect the connective tissues of the body, one of the most well-known being hypermobile EDS (hEDS). It is thought that there is a higher proportion of EDS in the ME/CFS community compared with the general population, but it is also worth noting that many with EDS are misdiagnosed with ME/CFS prior to an EDS diagnosis, likely because of the debilitating fatigue that accompanies symptoms.
So what exactly is EDS?
First lets start with what connective tissue is. Connective tissue is an absolutely essential component of the body, as the name suggests its role is to connect tissues (i.e.) keep tissues together, furthermore it is absolutely everywhere (basically everywhere where there is tissue). This means the symptoms of EDS are broad because it can effect connective tissues all over the body e.g. blood vessels, joints, skin. In the EDS connective tissue is weaker than normal, which can mean the body is essentially held together too loosely – leading to issue such as joint dislocation and subluxation (partial dislocation). EDS usually occurs as a result of an inherited faulty/mutated gene but in some cases the the faulty gene can occur in a person uninherited.
EDS is debilitating in general but also has a spectrum of severity, some of the rarer types can be life-threatening.
Signs/symptoms
Several types of EDS can have overlapping symptoms. The most common symptoms include:
- Joint hypermobility (increased range of joint movement)
- Excessively stretchy skin
- Fragile skin (breaks and bruises easily)
Individuals with EDS can experience many other symptoms/signs and complications such as, chronic fatigue (which can lead to a misdiagnosis of ME/CFS), chronic pain, joint dislocations/subluxations, digestive issues, problems with internal organs (e.g. aortic dissection – a serious and life-threatening complication).
Types of EDS
It is thought there are at least 20 genes associated with EDS. EDS occurs as a result of mutations in one or more of these genes. The specific genes affected, determines the particular type of EDS. There are actually 13 connective disorders that fall under EDS, some of which include:
- Hypermobile EDS (hEDS): most common form of EDS, mainly characterised by joint hypermobility (with frequent dislocations and subluxations) and milder skin involvement than other types. Note: for people who have problems caused by hypermobility but don’t have a condition that falls under EDS, they may be diagnosed with hypermobility spectrum disorder (HSD), which according to the NHS is treated in the same way as hEDS.
- Classical EDS (cEDS): greater skin involvement than other types, which is characterised by fragile hyperelastic (extremely elastic) skin that bruises and splits easily (especially in areas including forehead, chin, elbows, knees and shins, which are also common sites for scar formation)
- Vascular EDS (vEDS): rare type of EDS that affects the blood vessels and internal organs. It is often considered to be the most serious form, likely due to complications like organ rupture
Note: individuals with any of the types mentioned likely also have additional symptoms to the ones mentioned
ME/CFS and EDS
ME/CFS and EDS, particularly the hypermobile type (hEDS), are distinct but frequently overlapping conditions. Many individuals with hEDS have ME/CFS (Note: it is important to verify the presence of post-exertional malaise (PEM) – the hallmark of ME/CFS – rather than solely chronic fatigue which is highly prevalent in EDS). Similarly, amongst individuals with ME/CFS a higher proportion than in the general population show signs of joint hypermobility or have comorbid EDS. As with ME/CFS, dysautonomia, such as postural orthostatic tachycardia syndrome (PoTS) occurs frequently in EDS.
Management
There is no cure or specific treatment for EDS, however there are management options available for various symptoms, for example:
- Physiotherapy and occupational therapy – providing exercises to strengthen muscles supporting joints, aiding in joint stability; suggesting strategies and equipment
- Orthopaedics – providing instruments, such as braces or casting, for joint support and mobility aids such as a wheelchair
- Pain management
- Regular monitoring of heart and other internal organs to detect issues
- Extra support and monitoring during pregnancy and birth