A study by a research team led by Professor Elisa Oltra, who has previously worked on ME Research UK-funded projects relating to ME/CFS and human endogenous retrovirus (HERVs), has identified that certain markers in blood – including those relating to HERVs – were able to differentiate ‘post-COVID-19 condition’ – also known as long COVID – from healthy controls, those with ‘ME/CFS’, and those with fibromyalgia.
| What are HERVs? HERVs are viral fragments in the human genome – the entire set of genetic material, thought to be about 20,000 genes in humans – which are a result of immune responses to ancient viral infection affecting an ancient species or pre-human ancestors. Several health conditions, including lupus, rheumatoid arthritis, and multiple sclerosis, have been linked with high levels of HERVs. Research has shown that elevated levels of HERVs may also be found in people with ME/CFS, and those with long COVID. |
The study aimed to measure and compare circulating levels of a toxic HERV – “HERV-W ENV” – among 193 ‘females’ (males were excluded from the study to control for the potential impact of sex):
- 33 with ‘post COVID-19 condition’.
- 12 diagnosed with ME using the International Consensus Criteria (the research team referred to these participants as having ‘ME/CFS’).
- 42 diagnosed with fibromyalgia (FM) using the American College of Rheumatology.
- 60 who were diagnosed with both ‘ME/CFS’ and fibromyalgia.
- 46 healthy controls.
Importantly, those with ‘ME/CFS’, FM, and those who had a co-diagnosis of both ‘ME/CFS’ and fibromyalgia, received their diagnoses before the onset of the COVID-19 pandemic.
Results showed that HERV activation was identified in 48.5% of those with post COVID-19 condition – this was higher than in those with ‘ME/CFS’ (25%), FM (33.3%), in the co-diagnosis group (30%), and in healthy controls (8.9%).
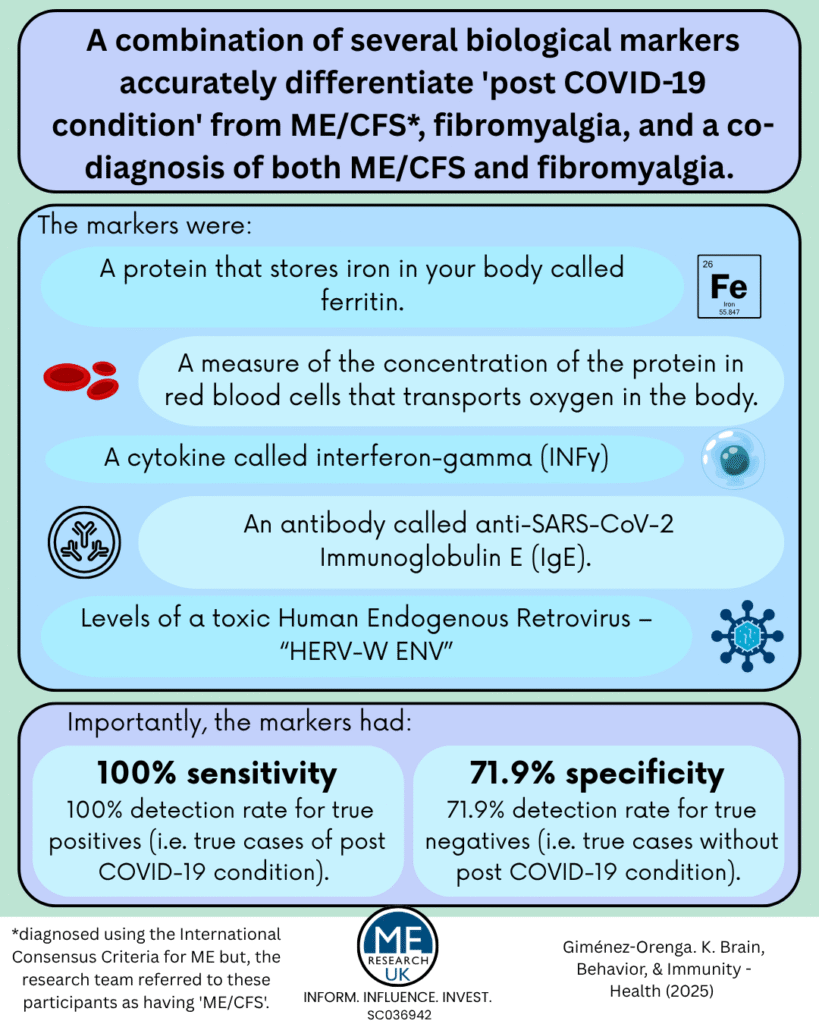
Interestingly, the researchers also found that using a group of biological markers – specifically; a protein that stores iron in your body called ferritin, a measure of the concentration of the protein in red blood cells that transports oxygen around the body (mean corpuscular hemoglobin concentration), a cytokine called interferon-gamma (INFγ) and an antibody called anti-SARS-CoV-2 Immunoglobulin E (IgE) – they were able to accurately distinguish those with post COVID-19 condition from all other participants in the study with:
- 100% sensitivity – meaning that the test could accurately detect ‘true positives’ – true cases of post COVID-19 condition – 100% of the time.
- 70.8% specificity – meaning that the test identified ‘true negatives’ – those who truly did not have post COVID-19 condition – 70.8% of the time.
When HERV-W ENV was also added to the group of markers, sensitivity remained the same, and specificity rose to 71.9%.
An important limitation of the study was that complete questionnaire data, and information on red blood cells was only available for 14 of the 33 people with post COVID-19 condition – the researchers noted that despite this small sample size for two of the biological markers, the investigation was still able to identify a “robust combination of markers capable of distinguishing post-COVID-19 condition”.
In the article it is noted that over half the people with ‘post-COVID-19 condition’ go on to fulfil ‘ME/CFS’ and/or fibromyalgia clinical criteria a few months following SARS-CoV-2 infection. The authors explain that this ‘co-diagnosis’ can pose significant challenges for healthcare systems. The biological markers identified in this study may provide a promising tool for stratifying people with post COVID-19 for individualised medicine programs.
The findings from this research build on the conclusions drawn by the team in an earlier paper, in which they suggested that:
- HERV-W ENV antigenemia and anti- SARS-CoV-2 IgE serology should be further studied to better characterize post-COVID-19 condition pathogenic drivers potentially differing in subsets of patients with various symptoms.
- Such biomarkers may serve to design therapeutic options for precision medicine in post-COVID- 19 condition.
Note : ME/CFS is a symptom-based clinical diagnosis not a mechanistic one. It is clear there is a high degree of shared pathophysiology between the ME/CFS and long COVID and the two diagnostic labels are not mutually exclusive.
Read more about Professor Oltra’s ME Research UK-funded work:
- Increased TTMV9 virus levels in immune cells from people with ME/CFS
- Could HERV expression be useful in the diagnosis of ME/CFS?
- Human endogenous retroviruses (HERVs) and long COVID
- Persistent HERV expression in patients with post-COVID symptoms
- The effect of activated HERVs and the associated immune response in severe ME/CFS