“Living with ME/CFS is unpredictable and exhausting. The symptoms – post-exertional malaise, brain fog, fatigue, pain, hypersensitivity, the list goes on – impact every aspect of life.”
Person with ME/CFS, 2025
ME Research UK-funded research suggests that in excess of 400,000 people in the UK have ME/CFS. This is more than the numbers of people living with HIV or multiple sclerosis. Furthermore, it is highly likely that this figure falls short because of misdiagnosis and delays in diagnosis.
According to research, people with ME/CFS are more limited than those with other illnesses (such as multiple sclerosis and other chronic conditions) in their ability to perform daily activities.
The physical symptoms of ME/CFS vary in severity between individuals, and even within the same individual over time. This is called disease heterogeneity, and is thought to be one of the biggest challenges faced by ME/CFS researchers.
ME/CFS can a have a major impact on a person’s ability to carry out normal activities, including everyday tasks, keeping a job, going to school, and taking part in family and social life.
“There is a constant fear that the disease will worsen or that the symptoms will never improve. As ME/CFS takes so much from those who live with it – relationships, access to education, employment, the ability to plan for the future – there is a constant sense of grief.”
Person with ME/CFS, 2025
Many people with ME/CFS are unable to work fulltime, and up to a quarter are house- or bed-bound.
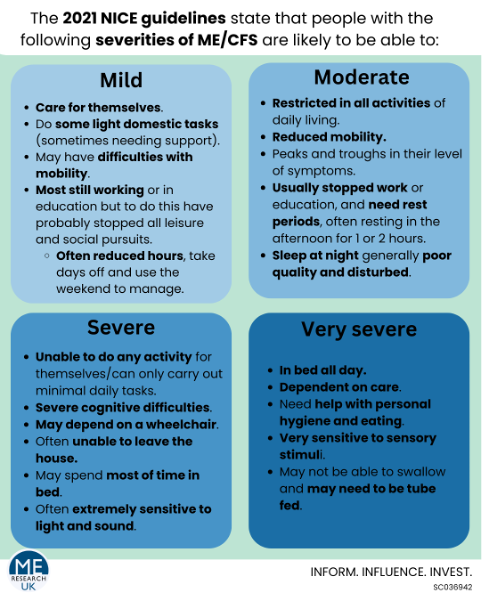
The different severities of the disease are reflected in the 2021 NICE guidelines.
Studies investigating the lived experiences of people with ME/CFS have highlighted how:
- people with ME/CFS have had to visit several healthcare providers to get a diagnosis or to have their symptoms recognised,
- people with ME/CFS experience post-exertional malaise (PEM),
- the most restrictive symptom of ME/CFS is PEM, followed by sensitivity to light, sound and smell (unfortunately, this study did not ask about the impact of cognitive difficulties).
Research into the lived experience of people with severe or very severe ME/CFS has found that the disease most significantly impacts function, nourishment, sleep and social isolation. This happens alongside a lack of professional understanding, prejudices, and challenges relating to the benefits system.
It is important to recognise that ME/CFS affects all social groups and all ages, including children. Women are more likely to be affected than men. Research has also suggested that, although those from Black and minority ethnic groups may be more likely to have ME/CFS, they are less likely to receive a diagnosis.
Some parts of the lived experience of ME/CFS may be different for different social groups. For example, there might be racial disparities in the diagnostic process for ME/CFS, or challenges to masculinity for men.
You can watch a series of videos covering different aspects of living with ME/CFS from a variety of perspectives in Natalie Boulton’s series, Dialogues for a neglected illness.