The 2025 IACFS/ME Virtual Research and Clinical Conference took place online between the 22-25th October 2025.
Speakers included Dr Leonard Jason, Prof. Sonya Marshall-Gradisnik, Dr Carmen Scheibenbogen, Caroline Kindon, and Dr Luis Nacul – all of whom have previously received research funding from ME Research UK – alongside Dr Suzanne Vernon, Dr David Goldstein, Dr Anthony Komaroff, and the chair of IACFS/ME, Dr Fred Friedberg.
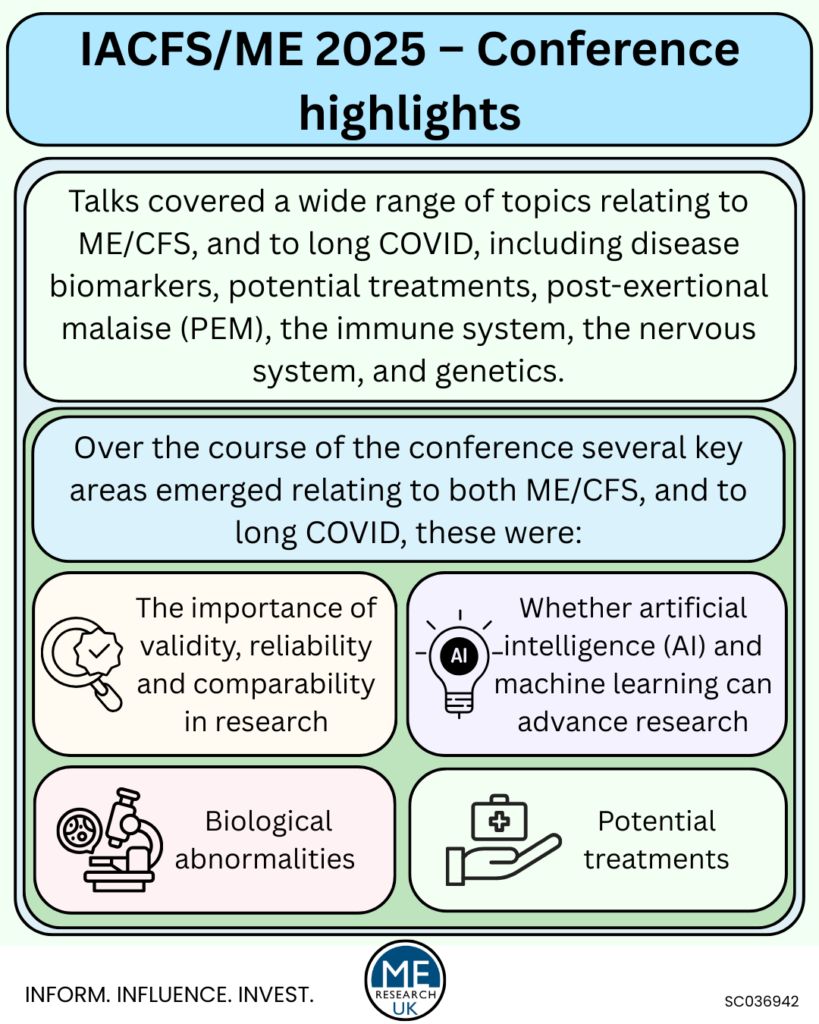
Talks covered a wide range of topics relating to ME/CFS, and to long COVID, including disease biomarkers, potential treatments, post-exertional malaise (PEM), the immune system, the nervous system, and genetics.
Over the course of the conference several key areas emerged relating to both ME/CFS, and to long COVID, these were:
- The importance of validity, reliability and comparability in research.
- Biological abnormalities.
- Potential treatments.
- Whether AI and machine learning can advance research.
The importance of validity, reliability and comparability.
Small sample sizes and lack of validation studies in ME/CFS research
In her welcome talk, Dr Nancy Klimas spoke about the importance of results being repeated across different studies; especially the need to repeat findings from small groups of participants, in larger more diverse cohorts. Regrettably, small sample size is a common limitation in research relating to ME/CFS due to the insufficient government-level funding available for large scale studies in many countries, including the UK and the USA. Validation studies, which look to repeat the findings observed in previous, often smaller, studies, are also hard to get funding for as they are not looking for novel findings. This means not only is the field held back by small sample sizes, but also by a lack of result replication.
Dr Klimas highlighted that study sample size is one of the notable differences between ME/CFS and long COVID research; while ME/CFS researchers have been “struggling to get the numbers up” for years, after just a couple of years, long COVID researchers are publishing papers based on “400, 5,000, 15,000” participants meaning the results are ‘very definitive’, so much so that Dr Klimas advised conference attendees to
“Watch very closely the [long COVID] science. Much of it validating the work that many of us [ME/CFS researchers] have done for may years, much of it focusing exactly on the paths that we had and have shown the similarities in the places where the two illnesses overlap and cross”.
Methodological consistency
Although not a new topic of conversation in ME/CFS research, presenters, including Professor Leonard Jason and Caroline Kindon, spoke about the need for accurate case definitions for ME/CFS, and for long COVID, to ensure that results from different studies are comparable. Additionally, in a talk on disease mechanisms, Prof. Sonya Marshall-Gradisnik highlighted limitations with research methods such as the lack of universal ‘animal model’ – where non-human organisms, like mice or zebrafish, are used to study human biological processes. Importantly, Prof. Marshall-Gradisnik noted that if all researchers were able to use one model to investigate disease mechanisms, results would be comparable. Instead, scientists must use samples of tissue, cells, serum, or plasma, or images from people with ME/CFS without knowing which one is the most reliable method, or even if the sample they are using provides the detail that is needed – an issue raised previously in a talk 2025 PolyBio Spring Symposium by Dr Amy Proal.
Reliability of research methods
Reliability of research methods were also touched upon; this refers to the consistency and reproducibility of measures or tools – such as questionnaires – used to capture information from participants. Many of the measures used in ME/CFS research are subjective – based on an individual’s perspective or lived experience – including those for post exertional malaise (PEM), the cardinal symptom of ME/CFS. Although capturing information on lived experience is important, there are limitations to subjective measures; for example, a scale rating levels of fatigue or pain may be perceived differently by different people (i.e. what one person perceives to be a pain level of four out of ten, might be a seven out of ten for another). Additionally, for some symptoms, especially PEM, there is no validated or ‘gold standard’ way to assess or capture information. This means that different measures are used across studies, again leading to reduced comparability and, regrettably, delays in research progress.
When considering the ‘best’ methods to use, researchers not only have to consider how useful the findings will be, but must balance this with the potential burden or risk to participants. When choosing which outcome measures to use, Drs Katharine Seaton and Natalie Eaton-Fitch specified eight factors which should be considered by researchers:
- Relevance to the research question and the patient benefit.
- Consistency over different measurements (across time or between researchers).
- Validity (whether an outcome measure captures what it was intended to measure).
- Responsiveness to real and meaningful changes over time.
- Whether the measure is feasible (is it practical within the resources, timeframe, and study design).
- Objectiveness (whether the measure captures the outcome without being influenced by factors such as personal feelings or opinions).
- How easy the measure is to interpret and apply in a clinical setting.
- Whether the measure minimises the burden or risk to study participants.
Summary
Overall, talks highlighted there is a clear need for consistency in the definitions and measurement tools used in ME/CFS, and in long COVID, research. Populations of participants should be clearly defined, and research methods – alongside their strengths and limitations in relation to the results of the study and how this might impact the interpretation of the findings – should be reported transparently.
Biological abnormalities
As expected at an ME/CFS conference, several different disease mechanisms were discussed, including decreased immune response, central noradrenergic deficiency, and transient Receptor Potential (TRP) ion channel abnormalities, and autoimmunity.
Decreased immune response
Research using data from the ME/CFS biobank, presented by PhD candidate Fang Fang Li, suggested that people with ME/CFS may have a decreased immune response, and that this may explain why they are more susceptible to pathogen reactivation.
Central noradrenergic deficiency
Dr David Goldstein spoke about ‘central noradrenergic deficiency’ in people with post infectious ME/CFS, and in those who have long COVID with PEM. Central noradrenergic deficiency is thought to have a negative impact on focus, alertness, energy, and mood. In the research Dr Goldstein presented, ME/CFS symptoms, including fatigue, correlated directly with decreased activity in the noradrenaline (also called norepinephrine) pathway. In the talk, it was postulated that low availability of the primary energy source in the body (adenosine triphosphate (ATP)) – something which has been associated with ME/CFS – may indirectly lead to these abnormalities.
Transient Receptor Potential (TRP) ion channel abnormalities
Professor Sonya Marshall-Gradisnik, who is involved in research funded by ME Research UK at the Griffith University in Australia, spoke about the potential link between Transient Receptor Potential (TRP) ion channel abnormalities and ME/CFS symptoms. The body is exposed to a wide range of physical and chemical stimuli – what Prof. Marshall-Gradisnik termed ‘threats/stressors’ – including (but not limited to) injury, temperature change, infection, chemicals, vibration, and allergens. TRP ion channels are responsible for detecting and coordinating the body’s response to these threats. Research has suggested that TRP ion channels may be impaired in people with ME/CFS. – interestingly, Prof. Marshall-Gradisnik highlighted that early-stage research from Matthias Löhn and Klaus Wirth has indicated that low dose naltrexone may act to restore TRP ion channel function in people with ME/CFS.
Autoimmunity
Former ME Research UK-funded researcher, Professor Carmen Scheibenbogen, spoke about the role of autoimmunity in ME/CFS, and explained how immune dysregulation could lead to brain fog, fatigue, pain, and exertional intolerance through dysfunction of the autonomic nervous system and the process in the body that produces and utilises energy (metabolism).
Potential treatments.
In his summary session on the final day of the conference, Dr Anthony Komaroff noted that there had been several talks on potential treatments for ME/CFS and for long COVID.
While the results of these studies are not yet conclusive – and in some cases the research is still underway – it is promising for people with ME/CFS, and for those with long COVID, that this early-stage research is now being done.
In fact, Dr Komaroff said:
“People are now studying treatments for ME/CFS which was essentially not the case for most of the last 40 years”
Some of the potential treatments discussed were:
Rituximab – A drug which is primarily used in the treatment of conditions such as rheumatoid arthritis and non-Hodgkin lymphoma, Dr Wakiro Sato explained that Rituximab acts by targeting a protein (CD20) found on the surface of B-cells in the immune system which produce the proteins – known as antibodies – which help to bind to pathogens and stop them infecting the body. More research is needed to assess whether this drug might be useful for people with ME/CFS.
Oxaloacetate – Oxaloacetate is a naturally occurring compound which plays a key role in the main energy production pathway in the body. When taken as a supplement, evidence suggests that oxaloacetate may work by increasing production of the primary energy source, ATP, for the cells of the body. Dr Susanne Vernon highlighted that as energy production is thought to be impaired in people with ME/CFS, and in those with long COVID, oxaloacetate may prove to be useful, although more research is needed.
Hydrogen enriched water – Dr Fred Friedburg spoke about a study investigating the potential usefulness of hydrogen enriched water for ME/CFS. Hydrogen enriched water is thought to work by boosting antioxidant activity in the body. Antioxidants are needed to combat ‘oxidative stress’ a state which occcurs when unstable oxygen-containing molecules, known as ‘reactive oxygen species’ or ‘free radicals’, are produced in excess and overwhelm the body’s antioxidant defences. While oxidative stress has been linked with inefficient energy use and decreased immune function in people with ME/CFS, more research is needed to assess the effectiveness of this treatment for the disease.
Hyperbaric oxygen therapy (HBOT) – HBOT is a medical treatment in which patients breathe in pure oxygen whilst inside a chamber with a higher-than-normal air pressure. The increased pressure pushes more oxygen into the lungs and then into the bloodstream, to be delivered to damaged or oxygen-deprived tissues to enhance healing. While HBOT is an established treatment for medical conditions such as diabetic foot ulcers and carbon monoxide poisoning, more research is needed to assess how safe and effective the treatment might be for people with ME/CFS.
Sleep medication use – Sleep issues are common in people with ME/CFS, with the NICE guidelines requiring the presence of ‘unrefreshing sleep and/or sleep disturbance’ alongside fatigue, PEM, and cognitive difficulties for a diagnosis of the disease to be made. Exploratory research presented at the conference suggested that many different medications are prescribed in the USA to treat sleep issues in people with ME/CFS. Results indicated that although sleep medications may help people with ME/CFS – in this case, either with their sleep or other ME/CFS symptoms – the self-reported effectiveness varied by drug, and the effectiveness may not make a meaningful difference to all people with the disease, meaning that more research is needed before any conclusions can be drawn.
“What might be helpful to one person might not necessarily be helpful to another person, or if it’s a side effect, it may not be worth it to another person” – Dr. Zachary McCann
Whether artificial intelligence (AI) and machine learning can advance research.
During the conference, the potential benefits of AI and machine learning for research into ME/CFS, and into long COVID, were underlined, for example, Dr. Anthony Komaroff predicted “AI to solve puzzles that have stumped us”.
AI refers to computer systems which can perform tasks that typically require human intelligence, such as learning, decision making, and reasoning.
Machine learning is a subset of AI that involves training an algorithm to make decisions or predictions based on data. Although there are many types of machine learning – including statistical models – linear regression and logistic regression – commonly used in research, the most popular type is a model that mimics the structure and function of the human brain known as ‘an artificial neural network’.
During the conference, Dr Natalie Eaton-Fitch discussed the potential application of machine learning in clinical trials, and suggested that in theory, machine learning could:
- Make drug discovery more efficient.
- Identify additional drug targets.
- Assist with the design of clinical trials and early stage (pre-clinical) studies.
- Predict individual side effects.
- Perform pre-trial safety profiling.
- Improve recruitment to trials.
Despite the potential for AI and ML in research investigating both ME/CFS and long COVID, Dr Eaton-Fitch highlighted the challenges faced by researchers including problems with small datasets, diversity (heterogeneity) of data, missing data, and the fact that results are often complex and difficult to interpret.
Takeaway messages
Throughout the conference, the importance of methodological rigor in ME/CFS research was highlighted. The pitfalls of methodological shortcomings were also discussed, both in general – such as small sample sizes in ME/CFS research noted by Dr Klimas – and specifically, in relation to PEM research where ambiguous definitions and poorly defined outcome measures were amongst the limitations discussed.
AI was discussed in a very positive light during the conference, but ME Research UK notes that caution must be applied. AI and machine learning are driven by existing data, much of which is not without limitations, including a lack of diversity, and biased samples – especially in the field of ME/CFS. These limitations should be taken into consideration when interpreting results generated through machine learning, and researchers should still strive to make their studies as inclusive as possible – for example, using patient and public involvement to develop recruitment methods that may be more accessible for those in underserved groups. This will increase the likelihood that the existing data and knowledge used by AI is representative of the population.
Another point worth noting is that during her talk, Prof. Schiebenbogen provided a ‘save the date’ for the next “Understand, Diagnose, Treat” conference which will take place in the 7th and 8th May 2026 in Berlin. This conference is usually also streamed online.
Finally, also at the IACFS/ME conference in 2025, to mark the 25th anniversary of the charity, ME Research UK sponsored the 2025 IACFS/ME virtual poster competition. Congratulations again to the well-deserved winners, Ms. Jolien Hendrix and Ms. Anne E. Gardella.